Maternal mortality rates in the United States have been rising at an unsettling pace, putting women’s health at risk during and following childbirth, according to recent data, and the number of pregnancy-related deaths has increased significantly over the past two decades. The United States has the highest rate of deaths for new mothers of any developed country, according to the Centers of Disease Control.
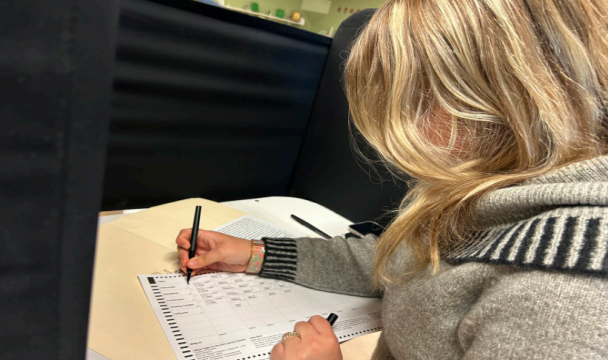
New statistics and medical trends were explained during a presentation titled “Preventing Maternal Mortality: The Educate to Advocate Symposium” on March 27 in Hislop Auditorium, held in collaboration with The Mohawk Valley Perinatal Network at the Neighborhood Center of Utica.
The event was led by keynote speaker and panelist Mary Siniscarco, Occupational Therapist and Associate Professor of Health Sciences at Utica University, with opening remarks from Dr. Kyrra Marchese, chair of the Health Sciences department at Utica University, Dr. Sarah Wolle, Associate Professor of Health Sciences assisted in moderating the event. The Health Science Student Society Executive Board members were also instrumental in event support.
According to the New York State Maternal Mortality Review Board, there are a variety of reasons for pregnancy-related deaths, such as: obesity, mental health concerns, substance abuse disorders and discrimination cases being the greatest cause of maternal death at 47%. Women of color face healthcare disparities and experience significantly higher maternal mortality rates due to systemic inequalities in healthcare access, quality of care and implicit bias among healthcare providers. Experts also pointed to racial inequities in low-income areas and women not being taken seriously when trying to address their health concerns. Black women are three times more likely to die from a pregnancy-related cause as compared to white women.
“A CDC statistic states more than 53% percent of maternal deaths occur from 7-365 days postpartum,” Siniscarco said. “ Shockingly, 80% of deaths are preventable.”
Also, postpartum depression can lead to suicidal thoughts and actions making suicide one of the leading causes of maternal death in the first year after childbirth.
“The hormonal changes, lack of sleep, and stress of new motherhood can worsen mental health, Siniscarco said. “Only 40% of women even know that birth can also cause postpartum post traumatic stress disorder which can occur from a traumatic birth experience.”
Panelist Joan Gallimo, a registered nurse and perinatal education specialist from the Mohawk Valley Perinatal Network at the Neighborhood Center INC, said the city of Utica offers a mobile crisis assessment team (MCAT) team that is designed to respond to mental health and substance use crises in the community, rather than requiring individuals to go to a hospital or emergency room, which can be helpful for women experiencing any form of pre/postpartum mental health concerns.
Many maternal deaths occur due to failing to recognize and act on urgent maternal warning signs such as a severe headache that won’t go away, dizziness, change in vision, fever, trouble bleeding, chest pain, fast heart rate, severe belly pain that won’t go away, severe nausea, vaginal bleeding or fluid leaking during or after pregnancy, swelling and pain in your leg or extreme swelling in hands or face and overwhelming tiredness. According to Siniscarco, it is of the “utmost importance to alert your medical provider if any of the above urgent maternal warning signs are experienced. Advocacy is key.”
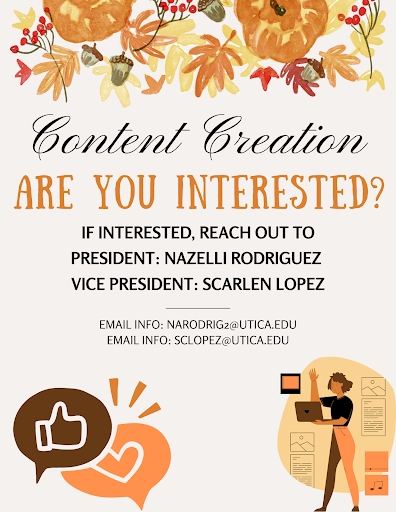
Sinisarco talked about needing a “Call to Action” at Utica University through the “Educate to Advocate” initiative where she will train interested students to deliver evidence-based presentations regarding urgent maternal warning signs to all women. You do not need to be a Health Science major or have a minor in Healthcare Advocacy and Navigation to actively participate in the “Educate to Advocate” initiative.
“Not only are you saving lives, you are developing your professional skills when you actively partake in the initiative,” Siniscarco said. “I just want motivated students who are willing to learn and make a difference. We need to encourage women to self-advocate.”
Other event panelists included, Dr. Rose Antilus, chair of the Department of Obstetric and Gynecology and Medical Director of Women’s Health at the Mohawk Valley Health System; Lois Sexton, Public Health Nurse with the Central New York Regional Office of the New York State Department of Health; and Megan Tyrrell, director of the Perinatal Regionalization Unit of the New York State Department of Health.
If interested in being part of the “Educate to Advocate” initiative, or to schedule an evidence-based Urgent Maternal Warning Signs presentation, please contact Professor Mary Siniscarco at [email protected] or (315) 792-3196.